Nape of head Acne Keloidalis Nuchae Treatment
Nape of head Acne Keloidalis Nuchae Treatment
Nape of head Acne Keloidalis Nuchae Treatment: Acne keloidalis nuchae (AKN) is a chronic inflammatory condition that affects hair follicles. A type of folliculitis, acne keloidalis nuchae is more severe. It first appears as bumps on the skin anywhere hair grows. These bumps are either papules — similar to pimples — or pustules, which are filled with pus. It is also known as keloidal folliculitis or nuchal keloidal acne.
SYMPTOMS OF ACNE KELOIDALIS NUCHAE
Symptoms of acne keloidalis nuchae usually begin on the back of the head and upper portion of the neck. Individual papules then join together horizontally, creating elevated, solid lesions that are greater than 1 centimeter in diameter known as plaques. Acne keloidalis nuchae areas lose hair due to the plaques, but there is limited hair growth surrounding the affected region. The aberrant hair shafts in areas affected by acne keloidalis nuchae break, and ingrown hairs result.
When acne keloidalis nuchae advances, the lesions grow larger. This causes pain, itching and a pus discharge in the region of those affected by advanced stages of acne keloidalis nuchae. African-Americans are mostly affected, followed by Asians and Hispanic/Latinos. It rarely occurs in Caucasians. Unfortunately, acne keloidalis nuchae is a permanent, chronic condition that is difficult to treat.
POTENTIAL CAUSES OF ACNE KELOIDALIS
Precisely what causes acne keloidalis nuchae in individuals remains unknown. The most probable hypotheses for the condition include:
Autoimmune Correlations
If the body’s immune system cannot properly decipher the difference between its own hair and foreign pathogens, it attacks non-threating hair shafts, follicles and sebaceous glands. The result is inflammation, and bacteria makes it worse.
Hair — especially when it is course and wavy — does not grow past the epidermis and instead grows down into the underlying dermis. This causes additional inflammation, followed by papules and pustules. This reverse growth triggers the body to respond to it as a wound and prompts an exaggerated healing response.
During the inflammation phase of the wound healing process, immune cells become conditionally deficient in energy and result in an over-recruitment of repair cells. In this “remodeling” of the injury, the rate of degradation of the extracellular matrix is slower than the stimulation of collagen formation, leading to adhesions, fibrosis and scar tissue.
Another hypothesis is that skin irritation from shaving or clothing cause hair shaft breakage. However, other studies found acne keloidalis nuchae was not caused by the autoimmune system.
Other Possible Triggers
Some physicians and scientists also theorize that bacterial infections, cyclosporine and mast cells may play a role in acne keloidalis nuchae. With bacterial infections, some classify it as a type of scarring alopecia in which bacteria-damaged hair follicles result in acne keloidalis nuchae symptoms.
Cyclosporine, an immune system suppressant drug, is another possible factor. It’s given to organ-transplant patients to prevent their immune systems from attacking the transplanted organ following surgery. Reports of Caucasian patients developing acne keloidalis nuchae after taking the drug have been reported.
Mast cells, when prevalent in the occipital region, are another possibility. Specialized cells of the immune system, a large number of them in this region may overreact to hair follicles.
Nape of head Acne Keloidalis Nuchae Treatment IN LOS ANGELES
Those affected with acne keloidalis nuchae have both non-surgical and surgical treatment options. Los Angeles clinics typically offer an array of methods to treat it due to dermatologists being familiar with the condition. The course of action depends on the stage of the condition.
Non-surgical Options:
- Radiation therapy
- Triamcinolone acetonide
- Cryotherapy
- Isotretinoin
- Topical steroids
- A topical antibiotic
- Isotretinoin
- Specialized shampoos
Surgical Options:
- Excision with trychophytic closure
- Excision with secondary intention healing
- A combination of excision and grafting
- Excision using a primary closure technique
- Electrosurgical excision
- Staged excision with primary closure
- Excision using a primary closure technique
Nape of head Acne Keloidalis Nuchae Treatment: Excision with Trychophytic Closure
Dr. Sanusi Umar, a board certified surgical dermatologist, is able to permanently address this condition rather than simply treat it. He combines his background in hair transplant surgery with his expertise on acne keloidalis nuchae. His Los Angeles-based clinic, located in Redondo Beach, has helped many who suffer from the condition when other treatments failed. Dr. Umar tailors his surgical procedures to individuals with a variety of techniques including:
- Posterior hairline migration
- Serial excisions
- Trichophytic closure
Despite the difficult nuances for addressing acne keloidalis nuchae, there are viable treatment options for each stage. For advanced cases, combined surgical excisions and trichophytic closure combinations can eliminate this condition. Nonetheless, always consult with a physician to determine the best plan for individual cases.
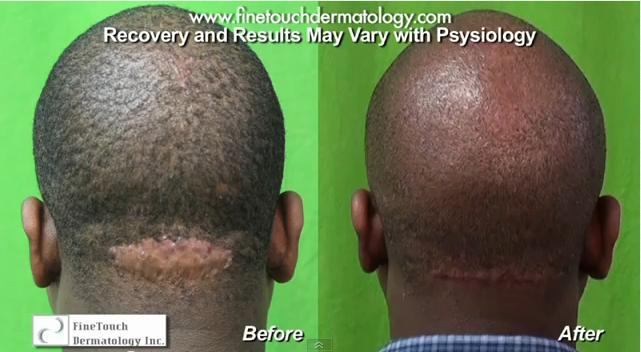
Acne Keloidalis Nuchae was removed through surgery to create an amazing improvement in this patient’s cosmetic appearance.*
…



Acne Keloidalis Nuchae Before and After Surgery
This patient had Acne Keloidalis Nuchae for six years. In the initial stages, the condition manifests as papules and pustules, which resembles acne on the back of the head. However in later stages, these lesions develop into tumor-like masses. This particular patient tried prescription medication for six months. However it did not help. He complained…
Read More